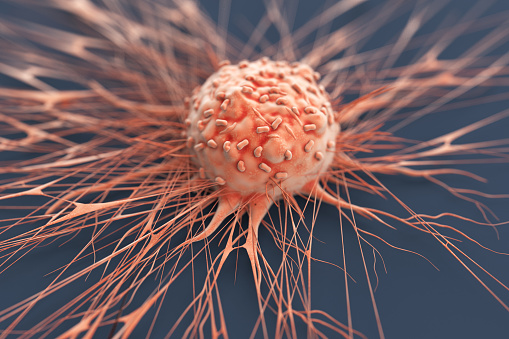
Cells Can Help To Treat Resistance In Prostate Cancer
Cells Can Help To Treat Resistance In Prostate Cancer. Throughout the whole course of the disease, from the early stages to the point of androgen independence. Where the tumour no longer responds to hormone restriction therapy. The researchers have detailed prostate cancer cell dynamics at a single-cell resolution.
Their research in mice, which was published in the journal eLife. Which shows that prostate cancer exhibits a proliferation of intermediate cells. Which is associated with treatment resistance and worse clinical outcomes in people. These cells are castration-resistant. Which explains why prostate tumours can resist hormone-related treatments since they can develop even in the absence of testosterone.
The most frequently diagnosed type of cancer and the second-leading cause of cancer-related deaths among men is prostate cancer. The likelihood of developing castration-resistant prostate cancer (CRPC). The lack of complete understanding of the cellular mechanisms behind the disease’s progression are both major contributors to this.
The two types of epithelial cells that make up the prostate gland epithelium. Which is a type of biological tissue that forms the surface of glands and organs. They are basal cells and highly-differentiated luminal cells (cells that have altered in form). However, it has previously been suggested that the luminal cells can develop into a more stem-like, castration-resistant intermediate.
Study Reveals
According to a Research in Molecular and Cellular Biology at the University of Washington in the US. The normal luminal cells may be able to transform into these progenitor cells under castrate conditions. There is evidence that these cells play a role in the early stages of prostate tumour growth. As well as treatment resistance in advanced malignancies, albeit this has not yet been verified in other models of CRPC.
Researchers created a “map of prostate cellular composition and evolution” over the course of the disease. By using a mouse model of CRPC in order to better investigate this.
Most individuals with advanced prostate cancer have inactive Pten. Which is a gene that codes for an enzyme that suppresses tumours. The scientists compared the populations of epithelial and non-epithelial cell types in Pten-deficient mice. Study with healthy mice using a method known as single-cell RNA sequencing.
They discovered basal, luminal, and luminal progenitor cells among other epithelial cell types in the prostates of healthy mice. They noticed a proliferation of luminal intermediate cells in the prostates of Pten-deficient mice, which were probably produced from basal cells, luminal progenitor cells, and developed luminal cells. This supports recent research in the field and demonstrates that basal cells can develop into intermediate cells after Pten ablation.
More research needed
The scientists also noticed that after hormone deprivation, malignant intermediate cells continued to grow, greatly increasing the variety of cells within a tumour (known as tumour heterogeneity). They showed that preventing protein production can limit this heterogeneity.
The scientists then worked to define the effects of this intermediate cell growth brought on by hormone deprivation. They found that a 5-gene signature is specifically concentrated in the intermediate cells. They demonstrated that the signature is linked to treatment resistance and subpar clinical outcomes using two datasets of bulk RNA-sequencing data from prostate cancer patients. A subset of metastatic human prostate cancer cells—tumors that can spread—also exhibit the signature’s enrichment, but not the originating tumour cells.
These results imply that a 5-gene signature established from prostate cancer animal models may be significant for understanding human illness. The existence of this gene signature may be a helpful prognostic indicator for predicting patient outcomes and treatment resistance. The Researcher request additional research to confirm the function of this signature and intermediate-like cell types in men with prostate cancer.
Additionally, their investigation showed that the prostate of mice lacking Pten is substantially enriched for immune cells that encourage the growth of tumours, resulting in a microenvironment that aids tumours in evading immune system suppression.
Cells involvement
Epithelial cells and fibroblasts, a type of cell that aids in the formation of connective tissue, attract pro-tumorigenic macrophages, a specialised cell type involved in the elimination of dangerous organisms. In order to overcome immunotherapy resistance in prostate cancer, it may be possible to stop the recruitment of tumor-associated macrophages.
According to senior scientists at the Department of Medicine and Genome Sciences (affiliate), University of Washington, “overall, our work highlights multiple epithelial and immune cell types that are crucial for prostate cancer initiation and progression, and sheds light on the interactions between specific cell populations that contribute to castration-resistance.”
“We want to support additional cancer research by offering a comprehensive, searchable database for researchers in the field. Therefore, we created a freely available, interactive website that enables researchers to conduct cell- and gene-specific inquiries over the entire set of 50,780 cells examined in our study.”